|
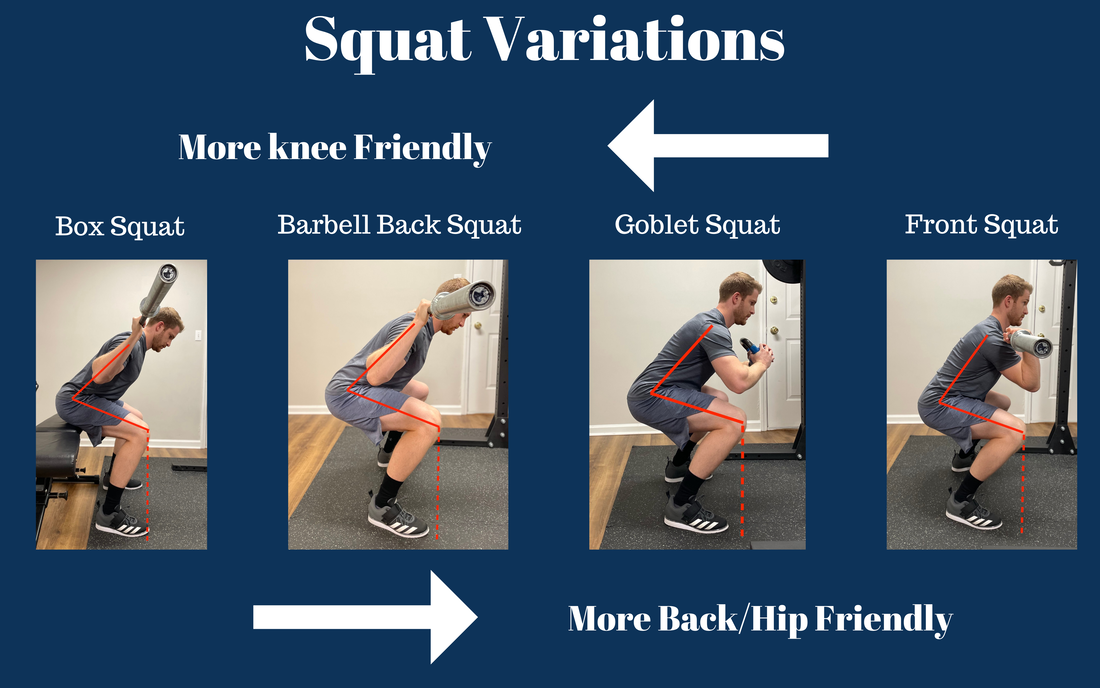
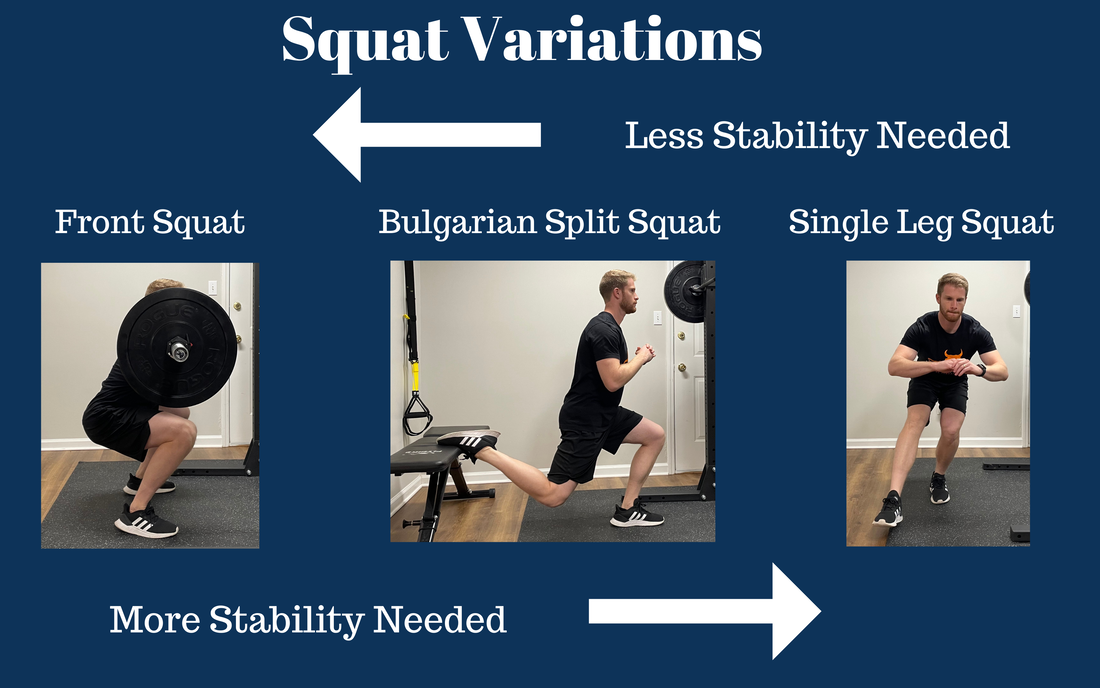
As mentioned in this article, the squat is a foundational exercise to strength training and physical therapy programs. There are many variations to the squat, and it can be overwhelming to try to decide what variation is right for you. When deciding on a squat variation, you should always begin with your end goal or reason for performing the squat. Some example goals may be to build muscle mass (hypertrophy), strength, muscular endurance, stability, power, reduce pain, or because my PT told me I should. Many people exercise because they want to feel and perform better. Squats are a compound (multi-joint) movement that is one of the most effective exercises for helping you do just that. Squats are also intimidating for many athletes, and they fear injury from them. Athletes fear injury from squats because of personal experience or stories of others who have experienced pain during and/or after performing them. So, they have good reason for fearing them, right? Kind of, but there is often a variation or modification they can perform relatively pain-free and safely. Also, many have pain due to compensations, which I addressed in my previous blog. In this article, I will cover the differences between the most common squat variations with an emphasis on how different squat variations affect joint stresses and require different levels of stability. This will give you confidence to continue squatting without fear of injury or in the case of pain/injury, to modify for success. In the sections below, I give detail to the reasoning behind the this infographic. This infographic is a generalization and simplification for the layperson's general benefit. For any astute biomechanics wizards out there, I understand that the science of calculating actual joint stresses during these variations is more nuanced and complex than this infographic. "Knee Friendly" Squat Variations The Barbell Back Squat The back squat tends to facilitate a more forward trunk lean with hips driven backwards further. This places more strain on the low back and hips. At the same time, there tends to be less forward translation of the shin (anterior tibial translation). The more the shin translates forward, the more shear force at the knee. This is how the “no knees over toes” phrase became popularized. The “knees over toes” during the squat debate is controversial in the fitness and physical therapy world. I tend to take a stance in the middle of the extremes on this debate. You cannot deny that more stress is placed on the knee with the knees translating over the toes. Inherently, this can lead to knee pain. What has failed to be demonstrated with research (and my clinical experience) is that allowing your knees to translate over your leads to higher rates of pain/injury. This does not give you free rein to purposely try to drive you knees over your toes with heavy weight and reckless abandon....yes, I see you "knees over toes" guy. If you are currently in knee pain, then modifying the squat variation to a more knee friendly variation may be needed in the short-term, The body is incredible at adapting. If you dose your training appropriately, then even heavy squats with allowing knees over your toes is likely safe. While I do not seem the harm in deep squats for many, unless you are a powerlifter or olympic weightlifter, then deep squatting is likely not necessary to accomplish your fitness goals. So, don't sweat it if it is not your thing. When someone is experiencing back or hip pain with squats with the absence of knee pain, I will often cue them to allow the knees to translate over their toes further to allow for the torso to stay more upright (less back/hip stress) as the descend into the squat. This is an example of how knowing the general joint stresses during squat variations can help you choose the right variation for your situation. For weightlifting athletes that enjoy squatting, the back squat is by far the most common. This is because it is much easier to add heavier load (weight) with the back squat. Heavier resistance means a larger muscle force required to accomplish he lift, leading to larger strength and hypertrophy gains. Heavier resistance inherently places more stress on your joints, so progress slowly and listen to your body if you start to experience pain. The Box Squat The box (or chair) squat is more of a sub-variation than its own distinct variation. What I mean is it can be performed with a barbell in a back squat fashion, any version of front rack (front squat variations), or goblet squat. The box often limits the depth (depending on the size of the box). The deeper you descend into the squat, the higher the stress placed on the knees; therefore, it is more knee friendly. The box also slows the movement down. Many people have a quick transition out of the bottom of the squat (“the hole”). Slower speeds reduce the rate of the load going through the body, further reducing the stress to the joints. If you perform them with slower speeds and reduced depth, the box squat becomes back, hip, and knee friendly. It is one of my favorites to start people with when recovering from injury! Back and Hip Friendly Squat Variations KeepGoblet and front squats both have the resistance in front of your body (“front rack”) compared to back squats that have weight behind the body. This facilitates a more upright torso. The upright torso typically places less stress on your back and hips, but more on the knees. These squat variations are a good way to start squatting when recovering from back pain or if you have a history of back pain. Front squats are easier to load heavy than goblet squats, which is a key factor when deciding the goal of your squat. The Foam Roller/Physioball Squat aka “The Safest Squat This squat is a variation of the wall squat. The purpose of the foam roller or physioball is to facilitate a smooth slide up and down during the movement. Why is this squat “the safest squat?” As you can see, the torso and shin angle are nearly vertical during this squat, greatly reducing shear force to the back, hip, and knee joints. This squat is knee, hip, and back friendly. Add an isometric hold at the bottom to feel the burn on the quads! Single Leg and Split Pelvis Squats So far, I have only covered bilateral squat variations. The two other main squat variations are split pelvis (ie: Bulgarian split squats) and single leg squats (ie: pistol squats). As you can see in the infographic, bilateral movements require the least amount of stability and single leg requires the most. The larger the base of support the less stability (balance) required. When I talk stability, I am not talking about structural integrity of the body. I am talking about the neuromuscular system’s ability to coordinate a movement in a skilled fashion. This is a complex process that is influenced by a myriad of factors, and for the purposes of this blog, we are not going to go deep here today. Split pelvis and single leg squats are often better for building stability while bilateral squat variations are better (for most people) for building strength and hypertrophy. This statement is also a generalization and simplification but tends to be true for many. For example, if I want quads like Arnold, it would probably be hard to do that with only single leg (or even split pelvis) movements because stability will eventually be the limiting factor instead of muscle fatigue. I should clarify that I am talking about free-weight movements. If you are using leg press or leg extension machines, it is easy to reach a strength and hypertrophy stimulus because machines eliminate the need for stability by providing it for you. If you are swaying all over the place like a bad dance move, then the stability challenge is too high, especially if strength instead of stability is the goal of the exercise. Besides a stability challenge, single leg and split pelvis squats allow for a lower load to be added before fatigue is achieved. A lower load is advantageous when currently experiencing pain (less load means less stress on the body) or programming thoughtfully to manage overall load to the body. In my clinical and fitness opinion, a well-rounded program that produces rock solid strength and stability will include bilateral, split pelvis, and unilateral squat variations Conclusion Squats are a crucial component to many physical therapy and fitness programs. If you are in pain or recovering from injury, knowing how different squat variations affect joint stresses and the different stability requirements needed can clarify which variation is right for your situation. If you currently in pain or still unsure of how to squat safely, schedule an appointment with our expert team today! Which squat variation/variations do you think are best for your goals and current health situation? Blog by: Dr. Dylan Michel, PT, DPT Disclaimer: Articles in the blog are not designed to be medical advice. If you have pain or an injury, I recommend seeing a healthcare professional. To schedule an appointment with Bull City Physical Therapy, visit our clinic page. References 1. Schoenfeld BJ. Squatting kinematics and kinetics and their application to exercise performance. J Strength Cond Res. 2010 Dec;24(12):3497-506. doi: 10.1519/JSC.0b013e3181bac2d7. PMID: 20182386.
0 Comments
The squat is one of the most popular exercises for many good reasons. The squat is very functional because we do it throughout our daily life (ie: picking objects off the ground, getting up/down from chair) and it mimics many sport movements. The squat is a compound movement (using multiple joints) that is great for building strength of the lower body, spine, and core musculature. It is estimated that over 200 muscles are activated in the squat. Instead of asking what muscles are activated in the squat, the better question is what muscles are not activated in the squat. What is normal?When I was in physical therapy school, professors would often say, “If you understand what normal is, you can figure out abnormal.” That being said, “normal” with squat technique varies depending on the goal of the squat, individual anatomy, and pain/injury history. In the video, I will review squat technique, keeping individual anatomy in mind. In the pictures below, I show two solid but different techniques for the squat. With "squat technique 1," you can see my torso is more upright, I am deeper in the squat, and my knees are moving further over my toes than "squat technique 2." The plates under my heels facilitate more ankle dorsiflexion, which allows for my tibia (shin) to translate further over my feet, resulting in a deeper squat and more upright torso. I am not advocating for squatting with plates under your heels necessarily, instead I used them to demonstrate a more upright torso for squat technique. My poor ankle dorsiflexion range of motion limits my ability to keep my trunk upright without plates under my heels or weightlifting shoes. The upright torso decreases low back and hip strain, but the knees translating further over my toes increases knee strain. This technique is typical with front squats and goblet squats. Squat Technique 1 Squat Technique 2 With "squat technique 2," the trunk is more flexed, which places more strain on the low back and hip and but less strain on the knees, making it more friendly for the knee. This technique is typical with barbell back squat, especially low bar back squats. I will cover squat variations in more depth in the next blog. Compensation #1: The "Butt Wink"The butt wink is when the low back flexes and the pelvis tilts backwards (posteriorly) at the bottom on the squat. When the body starts ascending out of the bottom of the squat (“the hole”), the low back then must transition from a flexed position back to neutral. Each time the low back transitions, this causes increased strain on the low back and under load, can lead to injury. The butt wink is only a compensation if it occurs before full depth and the movement is large. Everyone will have a some lumbar flexion if they squat down far enough, and that is normal. In the picture above, you can see that my low back is rounded at the bottom, causing the butt wink (large amount of lumbar flexion). Using my technique as an example, you can see my knees do not translate over my toes, decreasing the depth the butt wink occurs. Additionally, that is the maximum my hip will flex, which also limits the depth before my low back rounds. I have ankle and hip mobility issues, which is in large part due to my anatomy and not great for deep squatting. With consistent effort, many mobility deficits can be improved, but an individual's anatomy may cause a ceiling effect on how much it will improve. The butt wink is primarily caused by mobility deficits of your ankle and/or hips. Clinically, most often I see poor ankle dorsiflexion mobility as the primary culprit. Ankle dorsiflexion allows the tibia (shin) to translate over the foot, which is needed in the descent of the squat. In addition to ankle dorsiflexion mobility, hip flexion is needed at the bottom of the squat, and if it is lacking, the low back will round to compensate. Tight hamstrings, hip ligaments, and/or certain hip anatomy can all cause poor hip flexion mobility. The last reason for the butt wink is decreased lumbopelvic (low back and pelvis) stability. "Stability" is a combination of strength and motor control. Motor control is a scientific way of saying that the movement pattern is flawed. This is a result of training a poor movement pattern or improper timing and firing of muscles. Compensation #2 Exaggerated Forward Trunk LeanAs you can see in the picture, this compensation ends up looking like a combination of a hinge and a squat. People lean their trunk forward because they think they are squatting deeper, but in reality, their head is moving lower because of the trunk lean, which gives the illusion of a deeper squat. This compensation is almost always a motor control issue. The cue I like to give is “chest up.” If the compensation is due to a motor control issue, cueing with some mental effort should resolve the issue. Bad habits are hard to change. Allow time and consistent practice for the movement pattern to resolve. Compensation #3: Hips rise before chest (“good morning squat”)This video shows a compensation where the hips shoot up before the torso during the squat. I rarely see this compensation unless during a heavier loaded squat. This compensation can be a motor control issue or a quadriceps strength deficit. Compensation #4 Knees caving inwardThis video demonstrates the knee caving in (knee valgus) compensation. This compensation is because of a poor motor control, impaired ankle dorsiflexion mobility, and or hip and/or knee strength deficits. Compensation #5 Low back hyperextensionThis last compensation is primarily a motor control issue that people do not realize they are doing. When I see this, often it is because people are trying to keep their back straight (“neutral spine”) to avoid rounding their back and end up overcompensating with hyper-extending the low back. If I see this compensation, I teach a neutral spine and have the athlete practice maintaining that position during lighter weight squats before increasing the weight. Sometimes this compensation occurs with the "good morning squat" compensation. When the hips raise early, the low back can hyper-extend in an attempt to keep the torso upright. Final ThoughtsSquats programmed correctly and performed with good technique are safe and have a protective effect from injury. Mobility, strength, and motor control deficits can cause compensations that if unaddressed, can lead to pain and injury. Squatting through pain is not advised, and often there is an underlying impairment or training error that is causing the pain. I have heard many stories of people ditching squats because they have pain when that is usually not needed. Disclaimer: Articles in the blog are not designed to be medical advice. If you have pain or an injury, I recommend seeing a healthcare professional. To schedule an appointment with Bull City Physical Therapy, visit our clinic page. Author: Dr. Dylan Michel, PT, DPT References1. Aasa U, Svartholm I, Andersson F, Berglund L. Injuries among weightlifters and powerlifters: a systematic review. Br J Sports Med. 2017 Feb;51(4):211-219. doi: 10.1136/bjsports-2016-096037. Epub 2016 Oct 4. PMID: 27707741.
2. Kubo K, Ikebukuro T, Yata H. Effects of squat training with different depths on lower limb muscle volumes. Eur J Appl Physiol. 2019 Sep;119(9):1933-1942. doi: 10.1007/s00421-019-04181-y. Epub 2019 Jun 22. PMID: 31230110. 3. Schoenfeld BJ. Squatting kinematics and kinetics and their application to exercise performance. J Strength Cond Res. 2010 Dec;24(12):3497-506. doi: 10.1519/JSC.0b013e3181bac2d7. PMID: 20182386. 4. Steiner ME, Grana WA, Chillag K, Schelberg-Karnes E. The effect of exercise on anterior-posterior knee laxity. Am J Sports Med. 1986 Jan-Feb;14(1):24-9. doi: 10.1177/036354658601400105. PMID: 3752342. |
We accept the following insurance plans
Aetna, BCBS, cigna, uHC, UMR, Ambetter, medicare, Multiplan, Humana, and va choice
PT@BULLCITYPT.COM PHONE: 919.797.9588 FAX: 949.655.8592
Locations in Durham, Cary, and Charlotte to better serve you!
© 2023 Bull City Physical Therapy. All Rights Reserved.







 RSS Feed
RSS Feed


